The Inattentive, Impulsive and Hyperactive Child: Is Childhood Trauma Buried Amongst ADHD?
by Jessica Staniland, Clinical Psychologist - Psychologist BPsych (Hons) MPsych(Clinical)
December 2019
by Jessica Staniland, Clinical Psychologist - Psychologist BPsych (Hons) MPsych(Clinical)
December 2019

Do you have a foster or adopted child in your care who has come from a complex family background? Have you and your child been exposed to a potentially significant trauma at some point in your lives? Has your child been diagnosed with Attention Deficit Hyperactivity Disorder (ADHD) but there seems to be a piece of the puzzle missing? Does your child appear constantly hyper-aroused, anxious, or do they struggle with impulse control and emotional regulation?
These are questions to consider when determining whether your child may be experiencing a “trauma” reaction which may be either underlying or accentuating their ADHD.
These are questions to consider when determining whether your child may be experiencing a “trauma” reaction which may be either underlying or accentuating their ADHD.
A brief "run down" on ADHD
ADHD is a Neurobiological Developmental Disorder, meaning it’s related to the brain, runs in families, and impacts a child’s development and ability to learn. 1 in 20 children are diagnosed with ADHD at some point in their lives.
The main symptoms include impulsivity, hyperactivity, distractibility, poor concentration, racing thoughts and emotional reactivity. Interestingly, these symptoms can also be seen in chronic hyper-arousal after trauma.
The main symptoms include impulsivity, hyperactivity, distractibility, poor concentration, racing thoughts and emotional reactivity. Interestingly, these symptoms can also be seen in chronic hyper-arousal after trauma.
So, what is Complex Trauma?
Complex trauma refers to exposure to multiple traumatic events that are severe and pervasive, such as exposure to a natural disaster, exposure to domestic violence, and/or childhood abuse – physical, sexual, emotional or neglect of a child’s basic needs. What makes recognising complex trauma challenging is that it is subjective, and a child’s “traumatic stress” response depends on the:
Confusions around Trauma and ADHD
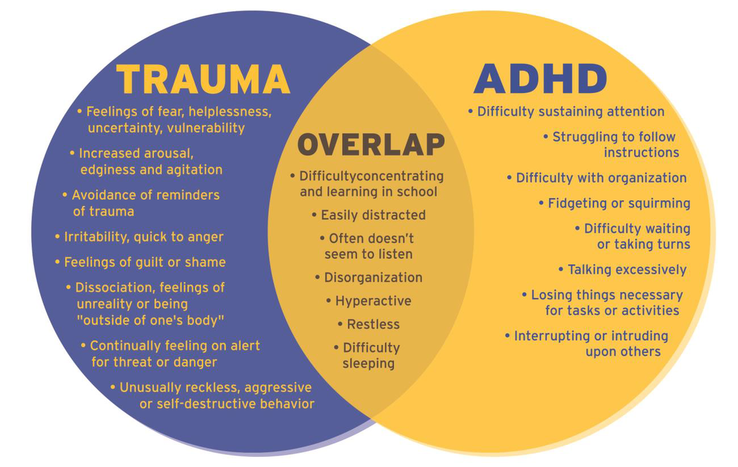
Below highlights the overlap between symptoms:
- Temperament of the child
- Developmental age when the trauma occurred
- Severity and duration of trauma
- Risk factors such as unstable home environment
- Protective factors such as a supportive family and consistent schooling environment
Confusions around Trauma and ADHD
Below highlights the overlap between symptoms:
Ref: The National Child Traumatic Stress Network, 2016
Why is there so much overlap?
- In response to trauma, a child’s developing brain can become programmed to “look out” for behaviour, activities or events that they perceive as threatening. This “hyper-vigilance” can often mimic hyperactivity and distractibility associated with ADHD.
- What may appear as inattention and “daydreaming” behaviour often seen in ADHD may actually be symptoms of dissociation or subconscious avoidance of trauma triggers.
- Intrusive thoughts, memories or other reminders of trauma may make children feel confused, agitated and nervous which may mimic impulsivity and aggression often seen in ADHD.
- Brain development studies for ADHD and child maltreatment show significant similarities in the areas of the brain that are affected (areas responsible for emotional regulation, decision making, memory, social processing and concentration).
Could my child have both Complex Trauma and ADHD?
Absolutely - if there has been significant trauma exposure. However, Complex Trauma is frequently a “missed” diagnosis because:
- Parents often under-report trauma in their children due to fear of blame or guilt.
- Clinicians don’t always ask questions about possible childhood trauma
- Complex Trauma is simply misdiagnosed as ADHD due to significant the overlap between presentations
So what can be done?
The earlier these difficulties are identified, the better the outcomes for your child.
- If you suspect your child may have been exposed to significant trauma, seek help from a professional as soon as possible. Your health professional is there to support you and your child.
- Trust your instincts. If you feel like your child’s diagnosis of ADHD doesn’t quite “feel right”, make sure you raise your concerns with your health professional and talk to your child’s teachers and other carers to determine if they have been witness to any significant traumatic events.
- Remember, children with ADHD and Complex Trauma backgrounds need:
- Consistency, predictability and routine within their lives - both at home and school
- Help to develop lasting, safe, and predictable relationships
- Key support people whom they feel comfortable going to, who understand them, and can empathise with them
- A sense of control through being provided limited choices
- To learn to build on their strengths and resiliency!
- Consistency, predictability and routine within their lives - both at home and school
Treatment Options
ADHD:
- Educational adjustments for learning in school
- Parent Behaviour Management Strategies delivered in a group or individual setting
- Stimulant Medication if recommended by a Developmental Paediatrician
- Therapy with a Psychologist who may utilise Trauma-Focussed Cognitive Behaviour Therapy (TF-CBT) and anxiety management techniques
- Sensory Regulation Activities as recommended by an Occupational Therapist
- Anti-arousal or anti-anxiety medications where necessarily, recommended by a Child and Adolescent Psychiatrist
Sources
ADHD in Children: Health Direct: https://www.healthdirect.gov.au/adhd-in-children
Making Space for Learning: The Australian Childhood Foundation: https://professionals.childhood.org.au/making-space-for-learning/
Is it ADHD or Childhood Traumatic Stress: A Guide for Clinicians (August 2016): https://www.nctsn.org/sites/default/files/resources/is_it_adhd_or_child_traumatic_stress.pdf
Trauma, Kids and ADDHD – Is there a Link? https://www.webmd.com/add-adhd/childhood-adhd/adhd-traumatic-childhood-stress
Costello, E.J., Erkanli, A., Fairburn, J.A., Angold, A. (2002). The Prevalence of Potentially Traumatic Events in Childhood and Adolescence. Journal of Traumatic Stress, 15(2), 99-112.
Hanbury, L. (2017). ADHD, Trauma and Neglect. How Do We Prevent Children Who Are In The Child Protection System From Being Misdiagnosed with ADHD? Improving Child Health Through Research Children’s Research Digest, 4(2).
Keeshan, B.R. & Strawn, J.R. (2014). Psychological and Pharmacological Treatment of Youth with Posttraumatic Stress Disorder: An Evidence-Based Review. Child and Adolescent Psychiatric Clinics, 23(2), 399-411.
Littman, E.B. (2009). Toward an Understanding of the ADHD –Trauma Connection. Drellenlittman.com
Perry (2006). Fear and Learning: Trauma related factors in the adult education process. New Directions for Adult and Continuing Education, 110, 21-27.
Van Der Kolk, B.A., Pynoos, R.S., Ciccheti,D.M., Cloitre, M., D’Andrea, W., Ford, J.D. et al. (2009). Proposal to include a Developmental Trauma Disorder Diagnosis for Children and Adolescents in DSM-V. Unpublished Manuscript.
ADHD in Children: Health Direct: https://www.healthdirect.gov.au/adhd-in-children
Making Space for Learning: The Australian Childhood Foundation: https://professionals.childhood.org.au/making-space-for-learning/
Is it ADHD or Childhood Traumatic Stress: A Guide for Clinicians (August 2016): https://www.nctsn.org/sites/default/files/resources/is_it_adhd_or_child_traumatic_stress.pdf
Trauma, Kids and ADDHD – Is there a Link? https://www.webmd.com/add-adhd/childhood-adhd/adhd-traumatic-childhood-stress
Costello, E.J., Erkanli, A., Fairburn, J.A., Angold, A. (2002). The Prevalence of Potentially Traumatic Events in Childhood and Adolescence. Journal of Traumatic Stress, 15(2), 99-112.
Hanbury, L. (2017). ADHD, Trauma and Neglect. How Do We Prevent Children Who Are In The Child Protection System From Being Misdiagnosed with ADHD? Improving Child Health Through Research Children’s Research Digest, 4(2).
Keeshan, B.R. & Strawn, J.R. (2014). Psychological and Pharmacological Treatment of Youth with Posttraumatic Stress Disorder: An Evidence-Based Review. Child and Adolescent Psychiatric Clinics, 23(2), 399-411.
Littman, E.B. (2009). Toward an Understanding of the ADHD –Trauma Connection. Drellenlittman.com
Perry (2006). Fear and Learning: Trauma related factors in the adult education process. New Directions for Adult and Continuing Education, 110, 21-27.
Van Der Kolk, B.A., Pynoos, R.S., Ciccheti,D.M., Cloitre, M., D’Andrea, W., Ford, J.D. et al. (2009). Proposal to include a Developmental Trauma Disorder Diagnosis for Children and Adolescents in DSM-V. Unpublished Manuscript.
We offer appointments with
Developmental Paediatricians (ages 5-17)
Child Psychologists (Young Adults)
Child and Adolescent Psychiatrists (ages 5-17)
See our full range of services.
Developmental Paediatricians (ages 5-17)
Child Psychologists (Young Adults)
Child and Adolescent Psychiatrists (ages 5-17)
See our full range of services.